Legionnaires’ Disease and Pontiac Fever are forms of Legionellosis, an infection caused by the bacterium Legionella. The number of annual cases in the United States has increased more than eightfold since the year 2000. The exact number is unknown, but there were nearly 10,000 cases in 2018. Legionellosis is rare but is many times more serious than the other recreational water illnesses (RWIs), including the very common rashes and ear infections caused by Pseudomonas. What is known is that improperly treated hot tubs are known to be one major source of human Legionellosis (Gerdes, et al, 2023).
The bacterium was named Legionella pneumophila after a 1976 outbreak in Philadelphia during an American Legion convention. During the outbreak, at least 239 people were infected. The outbreak began when a number of attendees developed serious pneumonia. The pneumonia did not respond to conventional medical treatment and 34 people died. Initially, it was not known whether the pneumonia was caused by infection or by chemical poisoning. After an extensive investigation, the illness was traced to previously unknown bacteria that were found growing in the HVAC system at one of the convention hotels.
Legionellosis is not spread by person-to-person contact. It is caused by inhaling airborne droplets of water containing Legionella bacteria. The diagnosis of Legionellosis requires specialized tests not routinely performed on persons with pneumonia or fever.
The most serious form of Legionellosis, Legionnaires’ Disease, is actually a severe form of pneumonia, and it can be fatal, especially to smokers and individuals with weakened immune systems who require prompt medical treatment or the prognosis can be dire. The second form of Legionellosis is Pontiac Fever, which is a mild infection and has symptoms similar to the flu. Individuals recover quickly from Pontiac Fever and do not usually require medical treatment.
WHERE DOES IT COME FROM?
Current studies show that Legionella bacteria are widespread in nature; more than 40% of all fresh waters contain Legionella bacteria. The bacteria most likely enter man-made systems, such as HVAC systems, water heaters, and hot tubs, via the fill water.
Legionella bacteria have a special lifestyle and unique nutritional requirements. They grow only when other microorganisms are present. The other microorganisms supply nutrients for the Legionella. Most of the time, the Legionella bacteria live as parasites inside of protozoa, especially amoeba. Sometimes Legionella grow as small colonies inside biofilm with other bacteria and fungi. Periodically, some of the Legionella break out of the protozoa or the biofilm and randomly swim in the water. It is these free-swimming Legionella cells that can cause Legionellosis.
Legionella are found only in wet locations, and they die when their environment dries out. The Legionella bacteria grow slowly at temperatures under 61 degrees Fahrenheit, but thrive when the temperature is between 90 and 106 degrees Fahrenheit. Operating conditions inside cooling towers, humidifiers, domestic hot water systems, and hot tubs are similar to the wet, natural habitat of Legionella. When these systems are not properly maintained, a significant biofilm will develop. This creates an environment where Legionella can grow and multiply into large colonies. If this happens, cooling towers, humidifiers, and showers may then broadcast fine droplets of Legionella- filled water into the air. If the droplets are the correct size, individuals can inhale the droplets. The droplets enter the lungs where they invade white blood cells and produce Legionellosis.
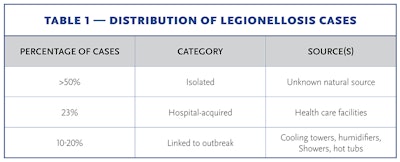
LEGIONELLOSIS CASES
Public health officials estimate that less than 10% of all cases are reported. The overall fatality rate is between 10 and 15%. The majority of Legionellosis infections are caused by accidental contact with the bacteria in natural bodies of water such as lakes or rivers.
The second largest source of infection is health care facilities such as hospitals and nursing homes. The fatality rate for these infections can be as high as 50%. This is not surprising in that these individuals have underlying health issues, which frequently include weakened immune systems. Engineered water systems, such as cooling towers and humidifiers, are the major source of infections.
A small number of cases have been traced to showers and hot tubs. In hot tubs, Legionella becomes trapped in the bubbles from aeration. When the bubbles break the surface, they burst and release fine droplets that contain the bacteria. Hot tub users and others in the vicinity inhale the airborne droplets into their lungs, where the bacteria produce an infection. It is likely the majority of infections from contaminated hot tubs are Pontiac Fever, the less severe form of Legionellosis. Legionella bacteria have not been found in hot tubs that are properly maintained. Swimming pools have not been linked with outbreaks.
EXAMPLES OF OUTBREAKS FROM HOT TUBS
The following well-publicized cases are typical Legionellosis outbreaks from hot tubs. According to CDC Surveillance Summary data, outbreaks of this type continue to occur as a result of inadequate sanitation.
Example 1. In 2018, an outbreak occurred at a hotel in New Hampshire. The source of a total of 94 confirmed, probable, and suspected illnesses was a 1,200-gallon indoor hot tub that was 20 years old. A permit had never been issued for the hot tub nor had it ever been inspected by the local department of health. The health department investigation did not find any record of treatment for the hot tub or any chlorine or bromine sanitizers at the hotel. The room holding the hot tub vented to the outside. Sixty of the 94 cases were in people several blocks away from the hotel that inhaled bacteria containing droplets exhausted by the fan (Daley, et al., 2022).
Example 2. In 2019, a total of 136 confirmed and 35 suspected cases of Legionellosis were reported after the North Carolina Mountain State Fair. This outbreak included 96 individuals who were hospitalized and four deaths. Because of the temporary nature of the fair, the investigation was not initiated before the fair had ended. The suspected source of the outbreak was a display hot tub that had not been properly disinfected and maintained (NC DHHS, 2020).
Example 3. In 2021, two individuals developed Legionnaires’ Disease from a second-hand hot tub. Both individuals were smokers. At least five other individuals used the hot tub but did not develop any medical symptoms. The investigation did not detect any sanitizer in the water but did detect Legionella bacteria in the household water system (Majury, et al., 2023).
HOW DO YOU CONTROL IT?
There are no convenient, easy, or inexpensive methods to detect if Legionella have colonized a venue. The most effective control method is to maintain a disinfectant in the water at all times.
Legionella bacteria in the water are killed by chlorine and bromine at normal use concentrations. There are no documented cases of outbreaks from hot tubs that have been properly and continuously sanitized. Legionella bacteria enter the hot tub with the fill water and are known to live inside garden hoses and domestic water systems. The introduced Legionella bacteria then invade and co-colonize the biofilm. All hot tubs have some amount of biofilm, with bacteria continuously leaving the biofilm and entering the water. When the sanitizer concentration is properly maintained, the bacteria in water are killed and do not cause illness. When the sanitizer is not properly maintained, bacteria leaving the biofilm and swimming in the water are still viable. These live bacteria are circulated by the pump and aerosolized by the blowers in the mists and droplets. Inhaling these droplets containing Legionella is how the bacteria enter the human lungs.
The U.S. Environmental Protection Agency (EPA) regulates products that control bacteria in swimming pools and hot tubs. Those products registered by the EPA as disinfectants/sanitizers have been proven to adequately control bacteria in swimming pools and hot tubs. A number of treatments are sold that claim to control bacteria but have not been registered by the EPA, and the ability of these products to control bacteria has not been independently verified. Therefore, these products may not provide the necessary control of disease-causing bacteria. The Pool & Hot Tub Alliance (PHTA) recommends that all hot tub and portable hot tub operators:
- Use an EPA-registered disinfectant/sanitizer. The product label will either use the word “disinfectant” or “sanitizer.”
- Follow the label directions.
- Maintain the concentration of the disinfectant/sanitizer specified on the label at all times.
- Maintain the pH between 7.2 and 7.8.
- Perform regular oxidation and water replacement.
- Frequently replace water in heavily used hot tubs and commercial hot tubs.
- Clean and refill lightly used residential hot tubs every three months.
If an outbreak is confirmed or suspected, the hot tub must be decontaminated at once.
- Close the hot tub immediately.
- Turn off the blowers.
- If the hot tub is indoors, make certain that air for the hot tub room does not circulate into the rest of the facility through the HVAC system.
- Replace the filter cartridges or filter media.
- Chemically clean the filter housing and all accessible areas. Disinfecting bathroom cleaners are suitable for most hot tubs. The area should be rinsed with tap water and the rinse water discarded before the hot tub is refilled.
- Decontaminate the hot tub (see Decontamination of Hot tubs and Wading (Kiddie) Pools Fact Sheet).